Same Evidence, Different Answers
Even when doctors are looking at the same research, they are often solving slightly different problems in their heads. Guidelines from credible groups help, yet those guidelines are not always identical, and they rarely capture the messy details of age, family history, access to care, and what you can actually stick with. On top of that, medicine changes faster than most people’s mental file cabinet, so you can hear old habits and newer evidence in the same week. Here are 20 topics where disagreement shows up in everyday appointments more often than most of us expect.
 National Cancer Institute on Unsplash
National Cancer Institute on Unsplash
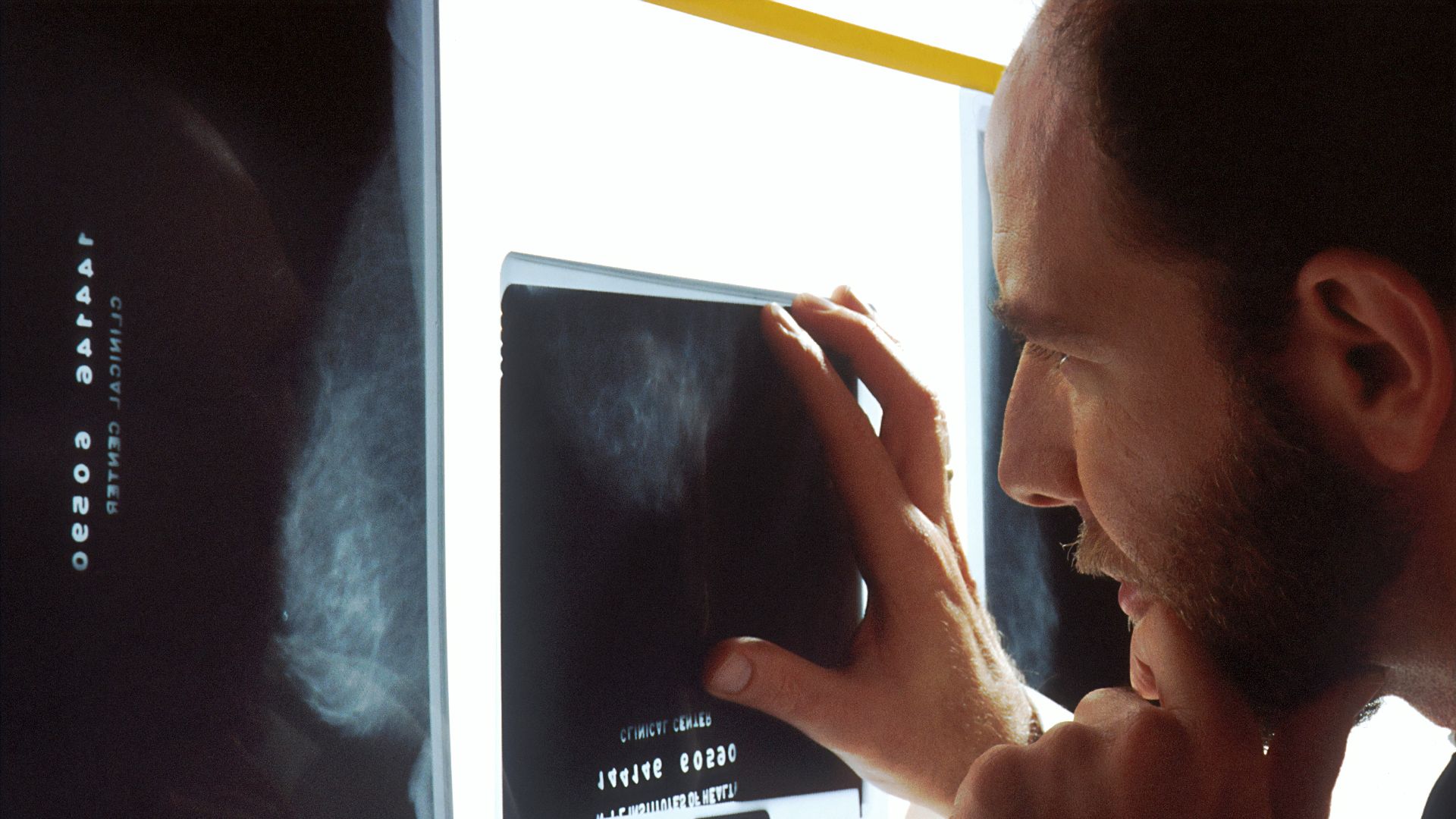
1. Mammogram Timing And Frequency
Even with clear guidance from the US Preventive Services Task Force recommending biennial screening mammography for women ages 40 to 74, some clinicians still favor annual screening for certain patients based on risk tolerance and local standards. Different doctors also weigh false positives and follow-up biopsies differently, especially for women with dense breasts or a strong family history.
 National Cancer Institute on Unsplash
National Cancer Institute on Unsplash
2. PSA Screening For Prostate Cancer
The US Preventive Services Task Force recommends individual decision-making for PSA-based screening in men ages 55 to 69, and that leaves room for real variation in how strongly a clinician nudges one way or the other. Some doctors emphasize the potential to catch aggressive cancer earlier, while others focus on the risk of finding slow-growing cancers that can lead to treatment complications.
 National Cancer Institute on Unsplash
National Cancer Institute on Unsplash
3. Colon Cancer Screening Approach
The US Preventive Services Task Force recommends colorectal cancer screening starting at 45 for average-risk adults, yet the method can still be a point of debate. Some clinicians lean toward stool-based tests as an easier on-ramp that patients actually complete, while others prefer colonoscopy because it can remove polyps during the same procedure.
4. Cervical Cancer Screening Schedule
For people ages 30 to 65, US Preventive Services Task Force guidance includes multiple acceptable pathways, including cytology every 3 years or high-risk HPV testing every 5 years, and that flexibility can translate into different clinical preferences. The American Cancer Society has also recommended starting at age 25 with primary HPV testing every 5 years when available, which can create variation in what different offices consider standard.
5. Whether Daily Aspirin Belongs In Primary Prevention
The US Preventive Services Task Force updated its recommendation in 2022, advising that starting low-dose aspirin for primary prevention in adults ages 40 to 59 with elevated cardiovascular risk should be an individual decision, and recommending against starting it in adults 60 and older. Some clinicians still have patients who have taken aspirin for years, and the disagreement often becomes about when to stop and how to weigh bleeding risk.
6. Who Should Start A Statin Before Any Heart Event
The US Preventive Services Task Force recommends initiating a statin for some adults ages 40 to 75 with risk factors and a sufficiently high estimated 10-year risk, while suggesting selective use for those at somewhat lower risk. Doctors differ in how they handle borderline cases, especially when family history, coronary calcium scoring, or medication hesitancy enters the picture.
7. What Counts As High Blood Pressure
US and European guidance has differed on diagnostic thresholds and treatment intensity, which can change how a borderline reading is labeled and managed. One doctor may treat 130 over 80 as a clear early-stage condition, while another frames it as a signal to monitor and focus on lifestyle changes unless other risks stack up.
8. How Aggressively To Lower Blood Pressure Targets
Even after a hypertension diagnosis, doctors can disagree on how low to aim, especially in older adults. Some prioritize tighter control to reduce stroke and heart risk, while others are more cautious if dizziness, kidney function changes, or falls are a concern in daily life.
9. A1C Targets In Type 2 Diabetes
The American College of Physicians has recommended aiming for an A1C between 7 percent and 8 percent for most patients with type 2 diabetes, rather than pushing for lower targets with medications that can cause harm. Other clinicians favor tighter control for selected patients who are younger, have fewer health problems, and can reach lower numbers without hypoglycemia or heavy treatment burden.
10. Whether Metformin Must Be The Starting Point
Metformin has long been a default first medication, yet newer drugs have shifted how some clinicians sequence treatment. The American Diabetes Association Standards of Care emphasize using certain GLP-1 receptor agonists or SGLT2 inhibitors for people with specific cardiovascular or kidney risks, and clinicians vary in how quickly they adopt that approach in routine practice.
11. Vitamin D Testing And Supplement Habits
Some doctors order vitamin D labs quickly and recommend supplements liberally, while others reserve testing for clear risk factors and focus on diet, sun exposure, and bone health basics. The US Preventive Services Task Force has recommended against low-dose vitamin D and calcium supplementation for fracture prevention in postmenopausal women, and it has also issued insufficient-evidence positions for broader routine supplementation decisions.
12. What To Do With Incidental Thyroid Nodules
Modern imaging finds thyroid nodules constantly, and clinicians do not always agree on how much follow-up is truly helpful. The US Preventive Services Task Force recommends against screening for thyroid cancer in asymptomatic adults, in part due to overdiagnosis concerns, yet incidental findings still create pressure to keep looking.
 Luiz Rogério Nunes on Unsplash
Luiz Rogério Nunes on Unsplash
13. Treating Mild Or Borderline Hypothyroidism
When thyroid labs are only slightly abnormal, some doctors start medication based on symptoms and patient preference, while others repeat labs and watch for spontaneous normalization. Disagreement often centers on how likely symptoms are to improve with treatment, and whether a daily medication becomes a long-term commitment without clear payoff.
14. Antibiotics For Sinus Infections
Some clinicians prescribe antibiotics early, while others use watchful waiting because many sinus infections improve without antibiotics. The CDC describes watchful waiting and delayed prescribing as common strategies, and doctors vary in how comfortable they feel using them depending on symptom severity and follow-up access.
15. Imaging For Low Back Pain
Patients often want an X-ray or MRI to make the pain feel more concrete, yet many guidelines caution against routine early imaging without red flags. Choosing Wisely recommendations endorsed by groups like the American Academy of Family Physicians advise against imaging for low back pain within the first six weeks unless red flags are present, and doctors differ in how they interpret those red flags in real appointments.
16. How Long To Stay On Acid-Suppressing Medications
For reflux, some clinicians aim to step down or stop proton pump inhibitors once symptoms are controlled, while others prioritize symptom relief and esophageal protection over long-term medication concerns. Disagreement often comes down to whether you have proven erosive disease, how often symptoms return, and how much lifestyle change is realistic.
17. Treating Uncomplicated Diverticulitis With Or Without Antibiotics
Many doctors were trained to use antibiotics routinely, and others now reserve them for selected cases based on newer evidence and the push to reduce unnecessary antibiotic exposure. The split tends to show up most for people who are stable, not immunocompromised, and have mild symptoms, where the risk-benefit calculation is less obvious.
18. Menopause Hormone Therapy Decisions
One clinician may recommend hormone therapy sooner for bothersome symptoms, while another is more cautious and focuses on the shortest effective duration for the right patient profile. The disagreement is rarely about whether symptoms are real, and more about timing, cardiovascular risk, breast cancer risk, and what outcomes matter most to you day to day.
19. Depression Treatment Sequencing
Some clinicians prefer starting with psychotherapy, others start with medication, and many combine both, depending on severity, access, and what you can sustain. Even when professional organizations publish evidence-based guidance, the on-the-ground decision still varies because availability, cost, and patient preference shape what is actually possible.
20. Weight-Loss Medication Versus Lifestyle-First Counseling
As newer anti-obesity medications have become more common, doctors disagree on when to introduce them and how to define readiness. Some see medication as a practical tool that reduces health risks sooner, while others worry about cost, side effects, long-term adherence, and whether supportive nutrition and activity plans are in place.